Learn what a clinical management plan is, why it matters in healthcare, and how to create one. Includes templates, real-life examples, and expert tips to improve patient care and communication across teams.
A Clinical Management Plan (CMP) is a critical document that streamlines patient care by clearly outlining diagnosis, treatment objectives, medications, monitoring, and responsible clinicians. Whether you’re managing chronic diseases, handling acute care, or navigating multidisciplinary treatment plans, a well-structured CMP ensures consistency, clarity, and compliance across healthcare settings.
In Canada and across many developed healthcare systems, clinical management plans are increasingly viewed as foundational to safe, effective, and patient-centered care. This guide will help you understand, develop, and apply CMPs effectively—whether you’re a clinician, healthcare administrator, or medical student preparing for regulated practice.
What Is a Clinical Management Plan?
A Clinical Management Plan is a formalized treatment framework agreed upon by a multidisciplinary team, outlining all aspects of a patient’s clinical care. It ensures that the healthcare team follows a coordinated approach, reduces communication errors, and documents accountability. In regulated settings, particularly for supplementary prescribing, a CMP is mandatory.
In Canada, CMPs are widely used in hospital systems, specialty clinics, and community health centers. The Canadian Medical Protective Association (CMPA) emphasizes proper documentation in clinical decision-making as a safeguard against malpractice and clinical ambiguity (CMPA – Documentation).
CMPs are especially crucial in scenarios involving:
- Chronic condition management (e.g., diabetes, hypertension)
- Post-operative care
- Mental health and psychiatric monitoring
- Oncology and palliative care
- Geriatric or complex multi-condition treatment planning
Key Components of a Clinical Management Plan
To serve its purpose, a CMP must be detailed yet accessible. Below is a breakdown of the typical elements included in an effective CMP:
| CMP Section | Details Captured |
|---|---|
| Patient Information | Full name, ID, age, diagnosis, medical history |
| Clinical Diagnosis | Confirmed or provisional diagnosis with supporting evidence |
| Treatment Objectives | Short- and long-term therapeutic goals |
| Medication Plan | Prescribed drugs, dosages, administration schedule, and responsible prescriber |
| Non-Pharmacological Interventions | Therapy, diet, rehabilitation, behavioral therapy |
| Investigations & Monitoring | Lab tests, imaging schedules, follow-up frequency |
| Roles & Responsibilities | Assigned clinicians, pharmacists, nurses involved |
| Review & Evaluation Timeline | Schedule for reassessment and necessary documentation updates |
| Contingency Plans | Escalation process, emergency contacts, and alternatives |
The National Institute for Health and Care Excellence (NICE) also outlines clinical guidance that reinforces the use of comprehensive treatment plans aligned with national protocols (NICE guidelines).
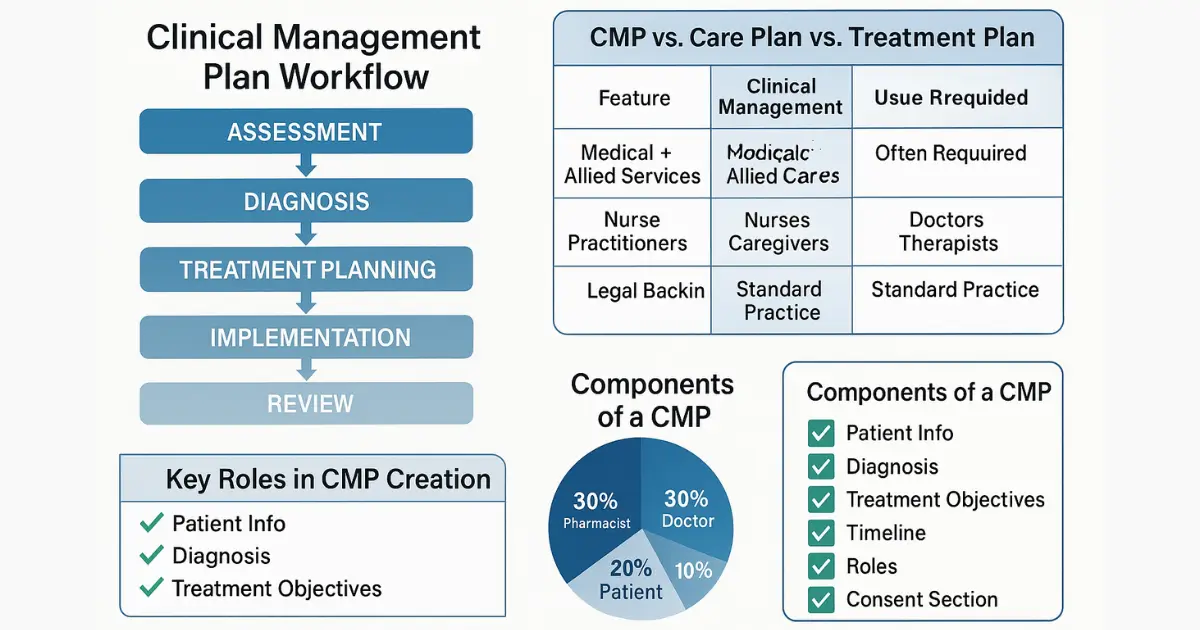
Why Is a Clinical Management Plan So Important?
Without a structured CMP, treatment can become fragmented, particularly when multiple specialists are involved. Studies show that care plans reduce medical errors, enhance communication, and improve adherence to evidence-based practices.
For example:
- A CMP ensures role clarity, so there’s no duplication of diagnostic tests or conflicting medication prescriptions.
- It fosters continuity of care when patients transition between acute and community settings.
- Documented CMPs have been shown to reduce preventable hospital readmissions by up to 25% in integrated health systems.
From a legal standpoint, properly maintained CMPs also serve as documented proof of due diligence in patient care, offering medico-legal protection.
How to Write a Clinical Management Plan: Step-by-Step Process
Creating a clinical management plan is not a one-size-fits-all task—it requires careful consideration of the patient’s medical status, treatment priorities, and multidisciplinary team roles. The process must be structured to promote consistency while allowing for personalized medical decision-making.
Step 1: Conduct a Comprehensive Clinical Assessment
Start by gathering detailed clinical information, including:
- Presenting complaints
- Past medical and surgical history
- Allergies and contraindications
- Current medications and treatments
- Recent diagnostic test results
This assessment forms the basis of the CMP. Tools like the Canadian Primary Care Assessment Tool (PCAT) help standardize this process in many provincial systems (Health Quality Ontario).
Step 2: Define Clear Treatment Goals
Goals should be specific, measurable, attainable, relevant, and time-bound (SMART). These goals align the entire care team and the patient toward defined clinical outcomes.
| Treatment Goal | Example |
|---|---|
| Short-Term | Achieve fasting blood sugar <130 mg/dL in 30 days |
| Medium-Term | Reduce HbA1c from 8.5% to <7% in 3 months |
| Long-Term | Prevent renal complications, maintain quality of life |
In patient-centred models, shared decision-making ensures these goals reflect the patient’s personal values and preferences.
Step 3: Outline Interventions and Responsibilities
Next, the interventions section of the CMP should be populated with both pharmacological and non-pharmacological treatments. Equally important is assigning responsibility to specific team members.
For example, in a diabetes management plan:
| Intervention | Responsible Clinician |
|---|---|
| Initiate metformin 500 mg daily | Nurse Practitioner |
| Nutrition counselling session | Registered Dietitian |
| Weekly blood sugar monitoring | Patient with support from RN |
| Monthly foot exam | Family Physician |
This clarity reduces duplication and ensures accountability.
Step 4: Schedule Follow-Up and Monitoring
A strong CMP includes a schedule for ongoing assessment and adjustment. Monitoring should be evidence-based and documented in a way that allows trend analysis over time.
- Blood work: Every 3 months
- Vitals and symptom check-ins: Biweekly
- Medication reconciliation: Monthly
- Team case review: Every 6 weeks
Platforms like Canada Health Infoway’s electronic health record systems support digital CMP integration for seamless communication and documentation (Canada Health Infoway).
Step 5: Add Contingency and Escalation Plans
Clinical conditions can change rapidly. A CMP must include clear protocols for escalation, especially in chronic disease or mental health settings. For instance:
- Blood sugar consistently >300 mg/dL → Immediate call to endocrinologist
- Mental health crisis → Crisis team notification and psychiatric consult
- Non-adherence to medication → Case manager intervention within 72 hours
Contingency planning ensures continuity even during deterioration or transition phases.
Legal and Regulatory Considerations in Clinical Management Plans
A clinical management plan (CMP) is not only a clinical document but also a legal instrument in many healthcare systems. In Canada, while there is no single federal CMP standard, provincial and territorial guidelines mandate robust clinical documentation practices. These ensure that care delivery is accountable, consistent, and auditable across public and private systems.
Legal Accountability and Clinical Governance
Healthcare professionals involved in a CMP share collective responsibility. Failure to document clearly—or to follow a mutually agreed treatment framework—can lead to adverse outcomes and medico-legal liability.
Key legal elements embedded in a CMP include:
| Legal Aspect | Requirement |
|---|---|
| Informed Consent | Documented patient agreement to interventions |
| Shared Responsibility | Clear designation of responsibilities among providers |
| Regulatory Compliance | Alignment with provincial guidelines and institutional protocols |
| Clinical Audits | CMPs must be retrievable for internal audits or external regulatory review |
Regulatory bodies like the College of Physicians and Surgeons of Ontario (CPSO) emphasize detailed clinical records and collaborative care standards (CPSO Record-Keeping Guidelines).
Role in Supplementary Prescribing & Advanced Practice
In the United Kingdom and increasingly in parts of Canada, supplementary prescribing allows qualified healthcare professionals (like nurse practitioners or pharmacists) to prescribe medication based on a pre-agreed clinical management plan.
For example:
- A nurse practitioner managing a patient with COPD can prescribe bronchodilators based on a CMP developed in consultation with a physician.
- A pharmacist in British Columbia may adjust insulin regimens under a CMP for diabetic patients, under collaborative prescribing models.
This structure is particularly significant in interdisciplinary care teams, where efficient role distribution enhances patient outcomes while maintaining regulatory compliance.
According to research by the Canadian Journal of Nursing Leadership, formalized clinical plans significantly reduce prescribing errors and improve continuity of care (Longwoods – Clinical Documentation in Nursing).
Documentation and Electronic Health Record (EHR) Integration
CMPs are increasingly integrated into electronic health records (EHRs) to ensure accessibility, interoperability, and auditability. Most modern systems allow for:
- Auto-alerts for medication conflicts
- Real-time updates by multiple team members
- Secure patient access and consent capture
- Timestamped edits and activity logs
| Feature | EHR Utility |
|---|---|
| Collaborative Editing | Physicians, nurses, and allied health professionals update in real time |
| Medication Alerts | System flags for allergies, interactions, and dosing conflicts |
| Version Control | Historical tracking of care plans and modifications |
| Secure Patient Portal | Patients can view and acknowledge their CMPs |
In Canada, leading platforms like TELUS Health and InputHealth offer customizable CMP modules that comply with federal privacy legislation under PIPEDA (Office of the Privacy Commissioner of Canada).
Real-World Examples of Clinical Management Plans in Action
Understanding the application of a clinical management plan (CMP) in real-life scenarios brings clarity to its value. In modern multidisciplinary settings—especially across Canada’s primary, acute, and community care systems—CMPs enhance communication, minimize risks, and improve patient outcomes.
Below are case-based examples demonstrating how structured CMPs function across different medical domains.
1. Chronic Disease Management: Type 2 Diabetes
Patients with diabetes often require coordinated care between primary physicians, endocrinologists, dietitians, and nurses. A CMP helps synchronize pharmacological, dietary, and behavioral therapies.
| CMP Feature | Details |
|---|---|
| Diagnosis | Type 2 Diabetes, uncontrolled HbA1c (9.1%) |
| Treatment Goals | Lower HbA1c to <7%, reduce fasting glucose to <130 mg/dL |
| Prescribing Plan | Initiate Metformin 500 mg BID, titrate every 2 weeks |
| Lifestyle Interventions | Monthly dietary reviews, physical activity counselling |
| Assigned Clinicians | PCP, Nurse Educator, Registered Dietitian |
| Review Schedule | Bi-weekly glucose logs, quarterly lab reviews |
In this case, the CMP ensures clear benchmarks and responsibilities. According to the Canadian Diabetes Association, collaborative care planning significantly reduces complication risks and healthcare costs (Diabetes Canada Guidelines).
2. Mental Health: Generalized Anxiety Disorder
In mental health care, consistency and continuity are paramount. A CMP allows for structured therapy schedules, medication review timelines, and crisis management strategies.
| CMP Element | Implementation |
|---|---|
| Diagnosis | GAD, confirmed by psychiatric evaluation |
| Pharmacologic Strategy | Sertraline 50 mg daily, review after 4 weeks |
| Psychotherapy | CBT sessions every 2 weeks, facilitated by licensed clinical psychologist |
| Risk Management | Emergency contact protocol, safety planning |
| Outcome Evaluation | GAD-7 assessment score every 4 weeks |
Integration of mental health CMPs into community mental health centers and EHR systems improves patient engagement and therapeutic success. This approach is promoted by the Mental Health Commission of Canada for enhancing primary care integration (Mental Health Commission of Canada).
3. Post-Surgical Recovery: Orthopedic Procedure
Post-operative care often involves multiple hand-offs between surgical teams, rehabilitation specialists, and community care providers. A CMP enables unified goals and tracking.
| Parameter | CMP Application |
|---|---|
| Surgery | Total Knee Replacement |
| Pain Management Plan | Oxycodone PRN, taper over 10 days; acetaminophen 1000 mg TID |
| Physiotherapy Schedule | Daily inpatient PT; weekly outpatient sessions post-discharge |
| Home Nursing | Wound inspection every 3 days; suture removal on day 14 |
| Monitoring | DVT prophylaxis adherence, infection signs, mobility milestones |
This level of care integration reduces complications and hospital readmissions. According to The Canadian Orthopaedic Association, structured post-op CMPs lead to faster recovery and higher patient satisfaction (COA Resource Library).
Common Traits of Successful CMP Implementations
Despite varying use cases, successful clinical management plans share several core attributes:
| Success Factor | Explanation |
|---|---|
| Clear Treatment Goals | Measurable objectives guide the care team |
| Defined Roles | Accountability across professionals |
| Evidence-Based Interventions | CMPs rely on best practices and clinical guidelines |
| Digital Accessibility | Integration with secure, user-friendly digital health records |
| Review Mechanism | Regular evaluation and timely updates to reflect patient progress or changes |
These best practices, when adopted consistently, result in more cohesive care delivery and improved patient outcomes.
Creating a Customizable Clinical Management Plan Template
To streamline care and improve documentation, many organizations develop clinical management plan templates tailored to their specialty or service model. Below is a customizable format that can serve as a foundation for most use cases:
| CMP Section | Details to Include |
|---|---|
| Patient Demographics | Name, age, sex, health ID, contact information |
| Diagnosis | Primary and secondary diagnoses with ICD-10 codes |
| Clinical Goals | Short-term and long-term measurable objectives |
| Interventions | Medication, therapy, diagnostics, referrals |
| Assigned Responsibilities | Clinician roles: who does what, and when |
| Monitoring Schedule | Timelines for lab reviews, physical assessments, and evaluations |
| Contingency Planning | Emergency contacts, adverse event handling protocols |
| Review Dates | Next review date and conditions under which plan must be re-evaluated |
Templates like this are often embedded into clinical decision support systems (CDSS) and EHRs. According to the Canadian Institute for Health Information (CIHI), standardization through CMPs improves both care quality and health system efficiency (CIHI – Health System Performance).
Key Takeaways and Best Practices
To truly leverage the potential of a clinical management plan, healthcare teams must go beyond documentation and embrace a culture of proactive, collaborative, and patient-centred care.
Top Clinical Management Plan Best Practices:
- Personalize: Tailor plans based on clinical, psychological, and social needs.
- Collaborate: Engage all relevant providers—nurses, pharmacists, specialists, social workers.
- Document Accurately: Every change or update must be time-stamped and attributed.
- Use Technology: Adopt EHR-integrated CMPs for improved coordination and reduced redundancy.
- Audit Periodically: Review CMP outcomes to identify patterns, gaps, and areas for improvement.
Health organizations like Accreditation Canada mandate integrated care planning as a part of their quality improvement frameworks to achieve better patient outcomes (Accreditation Canada Standards).
Final Thoughts
A clinical management plan is far more than a checklist—it is the blueprint of patient-centered care delivery. By aligning goals, structuring responsibilities, and promoting evidence-based decision-making, CMPs offer a strategic advantage to both providers and patients.
As Canada continues its shift toward team-based and digitally integrated care, CMPs will play a pivotal role in achieving outcomes that are safer, more efficient, and more responsive to patient needs.
FAQ
What is a clinical management plan?
A clinical management plan is a written healthcare plan designed by professionals to manage a patient’s condition effectively.
Who creates a clinical management plan?
It is usually created by a multidisciplinary team of healthcare professionals including doctors, nurses, and specialists.
Why is a clinical management plan important?
It helps ensure patient safety, clear communication, and well-organized treatment by setting defined goals and responsibilities.
Can a nurse follow a clinical management plan?
Yes. Nurses often use the CMP to guide care decisions and treatment delivery based on the predefined plan.
Is there a standard template for clinical management plans?
There is no single standard, but most templates include diagnosis, goals, treatments, assigned roles, and review timelines.
Can CMPs be integrated into EHR systems?
Yes, many modern healthcare facilities integrate CMPs into electronic health records for better tracking and coordination.
Do patients have access to their CMP?
In many healthcare systems, patients can access their CMP through patient portals to stay informed about their treatment.
Are clinical management plans used in mental health care?
Yes. CMPs are widely used in mental health to manage medication, therapy schedules, and emergency protocols.

About Author
Related Posts
Managed Clinical Networks Explained: How They Improve Healthcare Access, Quality & Coordination
Clinical Management Plan: Ultimate Guide for Healthcare Professionals in Canada
Why Seeing a Dietitian in Canada Matters: Expert Nutrition Advice for Your Health
Top Family Doctors in Edmonton: Your Comprehensive Guide