This complete guide explains Clinical Research Management Systems (CTMS) in simple terms. Learn about top tools, benefits, real examples, and how to choose the right CTMS for your clinical trials in Canada and beyond.
Clinical research has evolved into a complex, data-intensive process. With increasing regulatory scrutiny, decentralized trials, and multi-site collaborations, managing clinical studies manually is no longer practical or sustainable. That’s where a Clinical Research Management System (CRMS) or Clinical Trial Management System (CTMS) becomes a critical asset.
This guide provides a comprehensive look into CTMS, tailored especially for research professionals in Canada. Whether you’re a CRO, hospital research unit, or a biotech startup, this article will help you understand what CTMS is, why it matters in 2025, how it works, and how to choose the right system to streamline your clinical operations.
What is a Clinical Research Management System (CTMS)?
A Clinical Research Management System (CRMS) is an enterprise software platform designed to manage the operational, financial, and regulatory aspects of clinical trials. Commonly referred to as CTMS, it enables sponsors, sites, and contract research organizations to efficiently plan, track, and monitor clinical trial activities throughout their lifecycle.
In practical terms, a CTMS serves as the digital hub of a clinical study. It connects multiple stakeholders—including researchers, ethics boards, data managers, and regulatory bodies—through a centralized interface. By doing so, it ensures compliance, transparency, and real-time visibility into the trial’s progress.
Some core functions of a typical CTMS include:
| Feature | Functionality |
|---|---|
| Study Planning | Budgeting, forecasting, and milestone tracking |
| Site & Investigator Management | Site selection, onboarding, and document tracking |
| Participant Tracking | Enrollment, visit scheduling, and follow-up management |
| Financial Oversight | Grants, payments, and invoicing automation |
| Regulatory Compliance | eTMF integration, audit trails, and Health Canada compliance |
According to a detailed overview published by NIH’s National Center for Biotechnology Information, using a CTMS not only improves data integrity but also significantly reduces trial delays caused by operational inefficiencies.
Why is CTMS Critical in 2025?
The clinical trial ecosystem in 2025 is characterized by hybrid models, real-world data collection, and increasingly stringent compliance demands. Traditional, paper-based, or spreadsheet-driven trial management simply can’t keep up.
Some of the key trends making Clinical Research Management Systems indispensable in 2025 include:
- Remote/Decentralized Trials: Post-COVID-19, remote monitoring and decentralized patient recruitment are standard. CTMS helps track and manage decentralized workflows.
- Health Canada Regulations: Compliance with Health Canada’s guidance requires meticulous documentation and audit readiness.
- Multi-Site Coordination: CTMS platforms allow unified oversight across different trial sites with varying protocols and participant demographics.
- Real-Time Data Needs: Stakeholders demand immediate access to enrollment numbers, adverse event logs, and site performance metrics.
CTMS platforms streamline every stage of trial execution—from protocol development to final reporting—eliminating redundancy, human error, and compliance risk.
Clinical Management Plan: Meaning, Template, Examples & Guide for Better Patient Care
Key Features of an Effective Clinical Research Management System
Not all CTMS platforms are created equal. The effectiveness of a Clinical Research Management System depends on how well it aligns with the trial’s operational complexity, regulatory environment, and data management needs. Below are the essential features to look for in a high-functioning CTMS in 2025:
1. Centralized Study Start-Up Module
This component allows organizations to manage regulatory submissions, track start-up timelines, and ensure all pre-study milestones are met efficiently. It streamlines ethics board approvals, contracts, and site qualification, significantly reducing trial delays.
2. Real-Time Participant and Site Management
A robust CTMS provides real-time tracking of subject enrollment, visit scheduling, and retention activities. It also manages site performance metrics, helping sponsors identify underperforming sites early and take corrective actions.
3. Document & Compliance Management
Top-tier systems offer seamless integration with eTMF (electronic Trial Master File) and provide audit trails, version controls, and automated alerts for expiring documents. This is essential for maintaining compliance with ICH-GCP and Health Canada’s Division 5 regulations.
4. Budgeting & Financial Oversight
Financial transparency is a hallmark of a mature clinical operations strategy. CTMS platforms allow for automated budget planning, grant tracking, and investigator payments, reducing accounting errors and ensuring faster reimbursements.
5. Seamless Integration with Other Systems
CTMS platforms increasingly support integrations with EDC (Electronic Data Capture), IRB portals, and ERP systems. This reduces siloed data and ensures stakeholders are working from a single source of truth.
Here’s a comparative view of how these features differentiate basic tools from enterprise-grade CTMS:
| Feature Category | Basic CTMS | Advanced CTMS |
|---|---|---|
| Study Start-Up | Manual tracking via spreadsheets | Automated milestone tracking & alerts |
| Participant Management | Limited subject tracking | Real-time enrollment and visit updates |
| Compliance Tools | Basic document repository | eTMF integration + version control |
| Financial Management | Offline budget spreadsheets | Budget planning + automated payments |
| Integration Capabilities | Standalone system | EDC, eTMF, ERP integrations |
These features are not just “nice to have” — they’re rapidly becoming non-negotiable in regulated environments. According to a report from GlobalData Healthcare, organizations that implement a full-featured CTMS reduce trial costs by 12% and accelerate time-to-market by 18% on average.
Benefits of Using a CTMS
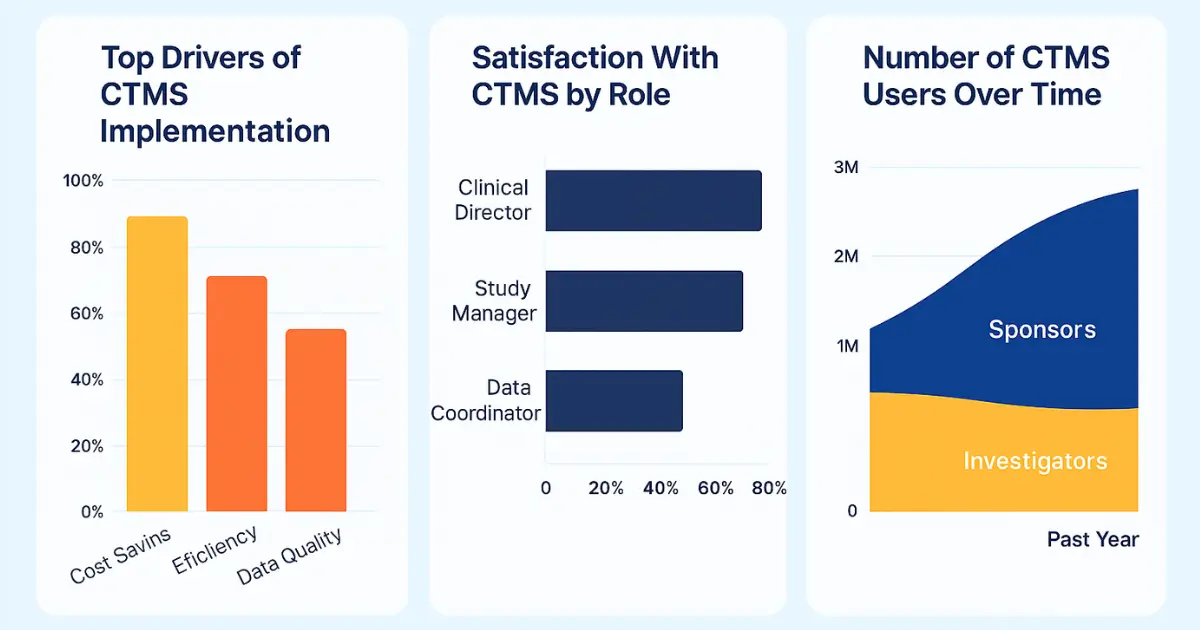
The adoption of a Clinical Research Management System brings measurable advantages across all phases of a clinical trial. For sponsors, CROs, and research sites, the benefits are both operational and strategic.
Improved Operational Efficiency
Manual data entry, site follow-ups, and fragmented communication are replaced by streamlined, automated processes. This leads to fewer errors, reduced rework, and shorter timelines.
Enhanced Regulatory Compliance
CTMS platforms enforce standardized workflows and maintain an audit trail, ensuring consistent compliance with local and international regulatory bodies. This is especially vital for Canadian sponsors adhering to Health Canada’s clinical trial requirements.
Financial Accuracy and Transparency
Managing complex budgets across multiple sites and phases is simplified through automated tracking and real-time reporting. This enables accurate forecasting, timely reimbursements, and clear financial oversight.
Scalable Growth
Whether you’re running one trial or 100, a good CTMS scales with your operations. It allows for the onboarding of new sites, integration of new study protocols, and expansion into international regulatory frameworks without compromising data integrity.
Clinical Supplies Management: A Simple Guide to Streamline Your Clinical Trials in 2025
Top Clinical Research Management Systems in 2025
The market for Clinical Research Management Systems is competitive and diverse, with platforms designed for everything from small site networks to global multi-phase trials. Here’s a curated comparison of the top-performing CTMS platforms in 2025, based on usability, features, compliance capability, and market adoption:
| CTMS Platform | Best For | Key Features | Pricing |
|---|---|---|---|
| Medidata CTMS | Large sponsors & CROs | Real-time analytics, global compliance support, eTMF integration | Custom quote |
| Veeva Vault CTMS | Enterprise-level clinical operations | Seamless EDC and eTMF integration, AI-based site selection | Tiered enterprise pricing |
| MasterControl | Mid-size pharma & quality-focused orgs | Document control, audit readiness, compliance modules | Starts at $50K/year |
| Florence eBinders | Research hospitals & investigator sites | Digital regulatory workflows, site enablement tools | Site-based subscriptions |
| RealTime CTMS | Small to mid-sized research sites | Scheduling, financial tracking, patient database | Starts at $299/month |
Each of these systems brings unique strengths to different segments of the clinical research ecosystem. For instance, Veeva Vault is favored for global scalability, while Florence excels in enabling research sites with limited resources to go fully digital.
According to a recent technology landscape review published by Clinical Leader, the ability to integrate with other clinical tech platforms—such as EDC, IRT, and ePRO—will define the CTMS leaders of the future.
How to Choose the Right CTMS for Your Organization
Selecting a Clinical Research Management System is a strategic decision that depends on multiple variables—trial complexity, team size, budget, regulatory jurisdiction, and more. Below are core evaluation criteria to help guide an informed decision:
1. Define Your Workflow Needs
Map out your trial workflows to identify the specific tasks you need the CTMS to handle—study start-up, site communication, data reconciliation, etc. This will help prioritize functionality over bells and whistles.
2. Assess Integration Capabilities
Your CTMS should not operate in isolation. Ensure compatibility with your EDC, lab information system, and document repositories. Seamless integration reduces data silos and accelerates decision-making.
3. Confirm Regulatory Readiness
If your trial is subject to Canadian regulatory oversight, the CTMS must meet Health Canada’s Part C, Division 5 compliance standards. Look for 21 CFR Part 11 certification, audit logging, and secure data handling features.
4. Evaluate Support & Training
Beyond software, the vendor’s onboarding, user training, and ongoing support offerings are critical to long-term success. Tools like RealTime CTMS offer self-paced training modules, while Medidata provides dedicated implementation consultants.
5. Request a Live Demo
Most reputable vendors offer live demos or sandboxes. Engage multiple stakeholders—clinical operations, finance, and regulatory affairs—in these demos to assess usability and alignment with internal processes.
Evaluation Checklist Table
| Evaluation Area | Questions to Ask |
|---|---|
| Workflow Fit | Does the CTMS support your current and projected trial workflows? |
| Regulatory Compliance | Is it validated and compliant with ICH-GCP and local regulations? |
| Integration Options | Can it connect with your EDC, eTMF, and finance systems? |
| User Experience | Is the interface intuitive for both sites and sponsors? |
| Vendor Support | What type of onboarding, training, and ongoing support is offered? |
Investing in the right CTMS will not only increase trial efficiency but also reduce risk exposure and enhance operational scalability across studies.
Real-World Use Case: CTMS in a Canadian Clinical Trial
To understand the practical value of a Clinical Research Management System, consider a mid-sized oncology research institute based in Ontario, Canada, running multiple concurrent Phase II and III clinical trials.
Challenge: The institute was managing over 25 study sites with fragmented communication, delayed regulatory document collection, and inconsistent reporting to Health Canada. Tracking subject enrollment and coordinating payments across institutions created administrative bottlenecks.
Solution: They implemented Veeva Vault CTMS, integrated with their existing EDC and eTMF solutions. With centralized dashboards, automated reminders, and real-time enrollment metrics, the organization streamlined the entire clinical trial lifecycle—from study start-up to close-out reporting.
Results:
- 37% reduction in study start-up time
- 50% faster document turnaround between PI and IRB
- Real-time Health Canada audit preparedness
This transformation was in line with broader trends highlighted by Applied Clinical Trials, which confirms that robust CTMS implementation directly correlates with reduced trial cycle times and improved regulatory confidence.
CTMS Compliance & Regulatory Considerations in Canada
One of the most important functions of a Clinical Research Management System is to help organizations maintain regulatory compliance throughout the study lifecycle.
In Canada, clinical trials are governed by Health Canada under the Food and Drugs Act (Part C, Division 5). This mandates:
- Documented informed consent
- Record retention for 25 years
- Ongoing adverse event reporting
- GCP-compliant procedures and inspections
Key Compliance Features to Look for in CTMS:
| Compliance Requirement | CTMS Support Function |
|---|---|
| 21 CFR Part 11 / Health Canada | Electronic signature validation, audit trails |
| eTMF Readiness | Document versioning, access controls, SOP integration |
| Inspection Preparation | Automated compliance dashboards, regulatory milestone tracking |
| Data Residency | Canadian-hosted servers or validated international data centers |
A compliant CTMS helps maintain transparency across sponsors, CROs, and regulatory authorities. For example, systems like MasterControl allow full visibility into trial documentation workflows, helping sites remain inspection-ready at all times. In fact, the Canadian Clinical Trials Asset Map also advocates for digitized systems that streamline data accuracy and accountability in trials.
In addition, organizations conducting international trials must consider alignment with ICH E6(R3), which encourages the use of risk-based monitoring and technology-supported quality management systems—capabilities well-supported by modern CTMS platforms.
Future of Clinical Trial Management Systems
The future of Clinical Research Management Systems lies at the intersection of automation, artificial intelligence, and decentralized trial support. The next generation of CTMS platforms will not just manage workflows—they will predict them.
Key Emerging Trends:
- AI-Powered Predictive Analytics
CTMS tools are beginning to incorporate machine learning to forecast site performance, recruitment bottlenecks, and budget variances. - Remote Monitoring Integration
With hybrid and virtual trials becoming the norm, integration with eConsent, telemedicine, and wearables is critical for continuity. - Real-World Data (RWD) Linkage
CTMS platforms will increasingly tap into electronic health records (EHRs) and claims databases to support post-market surveillance and outcomes research. - No-Code Workflow Customization
Sponsors will have the ability to configure protocols, user roles, and site workflows with no developer input—greatly reducing setup time. - Greater Focus on Patient-Centric Design
Expect interfaces and portals that are equally optimized for patient communication, not just operational staff.
By 2027, over 60% of global trials are expected to use AI-enhanced CTMS platforms, according to projections from MarketsandMarkets. The systems that adapt quickly to this future will be the ones defining the next era of trial innovation.
FAQs About Clinical Research Management Systems
What is the cost of implementing a CTMS?
The cost of a Clinical Research Management System can vary significantly based on the size of the organization, trial complexity, number of users, and integration needs. Small site-level systems may start at $300–$500/month, while enterprise-grade solutions can exceed $100,000 per year. Factors like data hosting preferences, compliance needs, and customization also influence pricing. Many vendors, such as Medidata and Veeva, offer custom pricing based on scope.
Who typically uses a CTMS?
CTMS platforms are used across the clinical research ecosystem:
- Sponsors (pharma, biotech)
- CROs (Contract Research Organizations)
- Academic Medical Centers
- Research Hospitals
- Independent Site Networks
The platform is designed to support diverse roles—clinical operations managers, regulatory coordinators, financial analysts, and site staff—all operating within a centralized digital environment.
How long does it take to implement a CTMS?
Implementation timelines vary. Basic CTMS platforms can be operational within 4–6 weeks, while more complex, enterprise-level deployments may take 3–6 months, including configuration, training, and systems integration. An effective implementation strategy often includes change management and stakeholder alignment as emphasized in Harvard Business Review’s technology adoption insights.
Can CTMS be used in non-commercial or academic trials?
Absolutely. Many academic and investigator-initiated studies use CTMS platforms to manage regulatory workflows, recruitment tracking, and compliance documentation. Tools like Florence and SimpleTrials cater specifically to smaller-scale research groups and academic hospitals.
Conclusion: Is a CTMS Worth It?
If you’re still managing clinical trials with spreadsheets, fragmented emails, and siloed systems, the answer is clear: Yes, a Clinical Research Management System is not only worth it—it’s essential.
From accelerating study start-up to maintaining regulatory compliance, and from improving data transparency to enabling real-time financial control, CTMS platforms empower organizations to run faster, safer, and more scalable clinical research operations.
In a highly regulated, competitive, and time-sensitive environment like clinical research, digital transformation is no longer optional. Whether you’re a sponsor overseeing multinational studies or a hospital managing a few investigator-led trials, the right CTMS will future-proof your research.
FAQ
What is a Clinical Research Management System (CTMS)?
A CTMS is a software tool used to manage the planning, tracking, and reporting of clinical trials in one centralized place.
Who needs a Clinical Research Management System?
Sponsors, research hospitals, CROs, and trial sites use CTMS to manage clinical studies and stay compliant with regulations.
What are the main features of a CTMS?
CTMS tools offer site tracking, budget management, document storage, regulatory compliance, and real-time reporting features.
How much does a CTMS cost?
Costs can range from $300/month for small teams to over $100,000/year for large organizations, depending on features and users.
Is CTMS required in Canada?
CTMS is not legally required, but it helps ensure trials follow Health Canada’s strict rules and documentation needs.
How does CTMS improve compliance?
CTMS systems keep detailed audit logs, store regulatory files, and send alerts for due tasks, keeping trials inspection-ready.
Can academic trials use CTMS?
Yes, many universities and hospitals use CTMS tools to manage investigator-led or student-supported clinical studies.
What is the difference between CTMS and EDC?
CTMS manages trial operations and documents, while EDC collects patient data. Both are often used together in clinical research.
How long does it take to set up a CTMS?
It usually takes 4–6 weeks for basic setups and up to 3–6 months for advanced integrations and full implementation.
Does CTMS support remote or hybrid trials?
Yes, modern CTMS platforms include tools for remote site monitoring, virtual patient tracking, and digital documentation.


About Author
Related Posts
How to Find the Right Gynecologist in Canada: A Step-by-Step Women’s Health Guide
Canada's Doctor Shortage: Causes, Impacts, and Solutions for a Healthier Future
How to Find a Specialist Doctor in Canada Without Long Wait Times (2025 Guide)
Women’s Health Clinics in Canada: Comprehensive Care for Every Life Stage